Services
Hernia
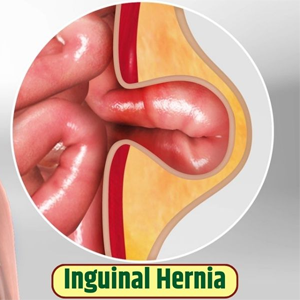
Inguinal Hernia : An inguinal hernia is a condition characterized by the protrusion of tissue, typically part of the intestine, through a weak spot in the abdominal muscles, specifically in the inguinal canal, located in the groin area. It is more common in men due to the anatomical structure of the inguinal canal. Symptoms often include a noticeable bulge in the groin, discomfort or pain during activities such as lifting, coughing, or straining, and a feeling of heaviness in the affected area. Inguinal hernias can be classified as direct or indirect, depending on how they develop. Indirect inguinal hernias are often congenital and occur when the inguinal canal does not close properly before birth, while direct inguinal hernias are acquired and usually result from wear and tear of the abdominal wall. Diagnosis typically involves a physical examination and may include imaging studies like an ultrasound or CT scan to assess the hernia's size and contents. Treatment usually involves surgical repair, either through open surgery or minimally invasive laparoscopic techniques. If left untreated, an inguinal hernia can lead to complications such as incarceration or strangulation, where the blood supply to the trapped tissue is cut off, necessitating emergency intervention.
Umbilical Hernia : An umbilical hernia occurs when a portion of the intestine or fatty tissue protrudes through the abdominal wall at the site of the umbilicus (belly button). This type of hernia is common in infants but can also affect adults, particularly those who are overweight or have experienced multiple pregnancies. In newborns, umbilical hernias are often congenital, resulting from a weakness in the abdominal muscles that fails to close completely after birth. Symptoms typically include a noticeable bulge near the umbilicus that may become more prominent when the baby cries or strains. In adults, the bulge may be accompanied by discomfort or pain, especially during activities that increase abdominal pressure, such as lifting or coughing. Diagnosis is usually made through a physical examination, and imaging tests like ultrasounds may be utilized to assess the hernia's size and contents. Most umbilical hernias in infants close on their own by the age of 1 or 2, but surgical repair is recommended if the hernia is large, painful, or persists beyond early childhood.

Incisional Hernia : An incisional hernia occurs at the site of a previous surgical incision in the abdominal wall, where the tissue weakens and allows internal organs or fatty tissue to protrude. This type of hernia can develop after any abdominal surgery, including procedures such as appendectomy, cesarean section, or open heart surgery. Factors that increase the risk of incisional hernias include obesity, poor wound healing, infection, and activities that put strain on the abdominal muscles, such as heavy lifting or chronic coughing. Symptoms often include a noticeable bulge near the surgical site, which may be more prominent when standing or during physical activity. Patients might also experience discomfort, pain, or a feeling of heaviness in the area. Diagnosis typically involves a physical examination and may be confirmed through imaging studies like ultrasound or CT scans. Treatment generally involves surgical repair, which can be performed through open surgery or minimally invasive laparoscopic techniques. The surgical procedure often includes reinforcing the abdominal wall with mesh to prevent recurrence. Recovery times can vary based on the extent of the hernia and the surgical approach used, but most patients can return to normal activities within a few weeks. If left untreated, incisional hernias can lead to complications such as incarceration or strangulation, making timely intervention essential.

Femoral Hernia : A femoral hernia occurs when tissue, often part of the intestine, protrudes through a weak spot in the femoral canal, which is located just below the groin. This type of hernia is more common in women, particularly those who are pregnant or have had multiple children, due to the anatomical differences in the pelvic region. Symptoms typically include a painful lump in the groin or upper thigh, especially when standing, lifting, or straining. Femoral hernias can be harder to detect than other types, as the bulge may be less visible. In some cases, individuals may experience discomfort or a feeling of heaviness in the affected area. Diagnosis usually involves a physical examination, and imaging studies like ultrasounds or CT scans may be employed to confirm the presence and extent of the hernia. Due to the risk of complications such as incarceration or strangulation—where the blood supply to the protruded tissue is cut off—surgical intervention is often recommended. Treatment typically involves repair through open surgery or minimally invasive techniques, using mesh to reinforce the abdominal wall and reduce the likelihood of recurrence. Recovery may vary, but many patients can return to normal activities within a few weeks, though care should be taken to avoid heavy lifting and strenuous activities during the healing process. Prompt attention to femoral hernias is crucial to prevent serious health complications.

Obturator Hernia : An obturator hernia occurs when tissue, typically part of the intestine, protrudes through the obturator foramen, an opening in the pelvic bone that allows nerves and blood vessels to pass into the thigh. This type of hernia is relatively rare and is more commonly found in older women, particularly those who are thin or have lost muscle mass. Symptoms of an obturator hernia can be subtle and may include groin pain, hip discomfort, or pain radiating down the inner thigh. Patients might also experience bowel obstruction symptoms such as nausea, vomiting, and abdominal distension, which can complicate diagnosis. Due to its atypical presentation, obturator hernias are often misdiagnosed, making prompt recognition challenging. Diagnosis typically involves a physical examination and imaging studies, such as CT scans or ultrasounds, which can help visualize the hernia and assess its size and contents. Surgical intervention is the most effective treatment, usually performed through open surgery or laparoscopy, and often includes the use of mesh to reinforce the area. Because of the potential for complications like incarceration or strangulation of the bowel, timely surgical repair is crucial. Recovery time can vary, but many patients can resume normal activities within a few weeks, although care should be taken to avoid strenuous activities during the healing process. Early diagnosis and treatment are key to preventing serious health issues associated with obturator hernias.

Ventral Hernia : A ventral hernia occurs when tissue, often part of the intestine, protrudes through a weakness in the abdominal wall, typically at the site of a previous surgical incision or due to muscle strain. This type of hernia encompasses various subtypes, including incisional hernias and umbilical hernias, and is often associated with factors such as obesity, aging, and previous surgeries. Symptoms usually include a noticeable bulge in the abdominal area, which may become more prominent when standing, bending, or lifting. Patients may also experience discomfort or pain, particularly during physical activities that increase intra-abdominal pressure. Diagnosis is generally made through a physical examination, with imaging studies like ultrasounds or CT scans used to assess the size and contents of the hernia. Treatment often involves surgical repair, which can be performed through open surgery or minimally invasive laparoscopic techniques. The surgical approach typically includes the use of mesh to reinforce the abdominal wall and minimize the risk of recurrence. Recovery times can vary depending on the size and complexity of the hernia and the surgical method used, but many patients can return to normal activities within a few weeks. Failure to address a ventral hernia may lead to complications such as incarceration or strangulation, making timely intervention critical. Early diagnosis and appropriate surgical management are essential for optimal outcomes and to prevent potential complications.

Epigastric Hernia : An epigastric hernia occurs when tissue, often part of the abdominal fat or intestine, protrudes through a weakness in the abdominal wall in the epigastric region, which is located between the chest and the umbilicus (navel). This type of hernia is typically small and can be present as a bulge or swelling in the upper abdomen. Epigastric hernias are more common in men and can occur at any age, often developing due to factors such as obesity, aging, or previous abdominal surgeries. Symptoms may include localized pain or discomfort, especially when straining or lifting, and patients might notice a small, soft lump in the area. Unlike some other hernias, epigastric hernias may not always be accompanied by significant symptoms, making them less noticeable in some cases. Diagnosis generally involves a physical examination, and imaging studies like ultrasounds or CT scans can be used to confirm the presence of the hernia and evaluate its contents. Treatment typically involves surgical repair, which can be performed through open surgery or laparoscopic techniques, often using mesh to strengthen the abdominal wall. Recovery times vary, but many patients can return to regular activities within a few weeks post-surgery. While epigastric hernias are not usually life-threatening, they can lead to complications such as incarceration or strangulation if left untreated. Therefore, prompt diagnosis and appropriate surgical intervention are important for preventing potential health issues and ensuring optimal recovery.

Lumbar Hernia : A lumbar hernia occurs when tissue, often part of the intestine or fatty tissue, protrudes through a weak spot in the muscles of the lower back, specifically in the lumbar region. This type of hernia is relatively rare and can occur in two main forms: congenital, resulting from a developmental defect, or acquired, often due to trauma or significant strain on the back muscles. Symptoms typically include localized pain in the lower back, which may radiate to the legs, as well as a visible lump or bulge in the lumbar region that may become more pronounced when standing or straining. Patients might also experience discomfort during physical activities, particularly those involving heavy lifting or twisting motions. Diagnosis usually involves a thorough physical examination and imaging studies like MRI or CT scans to assess the extent and nature of the hernia. Treatment options generally include surgical repair, especially if the hernia is causing significant pain or complications such as nerve compression. Surgical procedures may involve open surgery or laparoscopic techniques, with mesh often used to reinforce the abdominal wall. Recovery times can vary based on the complexity of the surgery and the patient's overall health, but many individuals can return to normal activities within weeks. While lumbar hernias are not as common as other types, timely diagnosis and intervention are crucial to prevent potential complications, such as chronic pain or impairment of nearby structures. Early management can lead to better outcomes and improved quality of life for affected individuals.

Pelvic Hernia : A pelvic hernia occurs when tissue, typically part of the intestine or fatty tissue, protrudes through a weakness in the pelvic floor muscles or the surrounding structures. This type of hernia is less common than others, and it can be classified into various subtypes, including obturator hernias and perineal hernias. Pelvic hernias are often associated with factors such as obesity, pregnancy, and chronic conditions that increase intra-abdominal pressure. Symptoms may vary depending on the specific type of pelvic hernia but often include discomfort or pain in the pelvic region, a noticeable bulge in the groin or thigh, and symptoms of bowel obstruction, such as nausea or vomiting. Patients might also experience urinary issues or changes in bowel habits, depending on the hernia's size and location. Diagnosis typically involves a physical examination and imaging studies like CT scans or MRIs to assess the hernia's nature and extent. Surgical intervention is usually recommended, particularly if the hernia is symptomatic or at risk of complications like incarceration or strangulation. Surgical repair can be performed using open or minimally invasive techniques, with mesh often utilized to reinforce the pelvic floor. Recovery times can vary based on the surgical approach and the patient’s overall health, but many can resume normal activities within a few weeks. Early recognition and management of pelvic hernias are crucial to prevent complications and ensure optimal recovery. With appropriate treatment, patients can achieve significant relief from symptoms and improve their quality of life.

Spigelian Hernia : A Spigelian hernia is a type of abdominal hernia that occurs through a defect in the Spigelian fascia, which is located between the rectus abdominis muscle and the lateral abdominal muscles. This hernia is relatively rare and often goes unnoticed until it becomes symptomatic. It can occur at any age but is more commonly found in adults. Symptoms typically include a noticeable bulge in the lower abdomen, often accompanied by localized pain or discomfort, especially during activities that increase abdominal pressure, such as lifting or straining. Unlike other types of hernias, a Spigelian hernia may not always present with a visible lump, making diagnosis challenging. Diagnosis generally involves a physical examination and imaging studies, such as ultrasounds or CT scans, to confirm the presence of the hernia and assess its contents. Due to the potential risk of complications, such as incarceration or strangulation, surgical intervention is often recommended. Surgical repair can be performed through open or laparoscopic techniques, with the use of mesh to reinforce the abdominal wall. Recovery times vary, but many patients can return to normal activities within a few weeks after surgery. Early detection and management of a Spigelian hernia are crucial to prevent serious complications and improve patient outcomes. With appropriate treatment, individuals can experience significant relief from symptoms and restore their quality of life.

Hiatus Hernia : A hiatus hernia occurs when part of the stomach protrudes through the diaphragm into the chest cavity via an opening called the hiatus. This condition is more common in older adults and can occur due to factors such as age, obesity, and increased abdominal pressure from pregnancy or heavy lifting. There are two primary types: sliding and paraesophageal. Sliding hiatal hernias are more common and occur when the stomach and the section of the esophagus that joins the stomach slide up into the chest. Paraesophageal hernias, although less common, can be more serious as they involve part of the stomach pushing through the hiatus alongside the esophagus. Symptoms may vary and can include heartburn, regurgitation, difficulty swallowing, chest pain, and in some cases, shortness of breath. Many individuals with a hiatus hernia may remain asymptomatic, but those who experience symptoms often find them exacerbated by lying down or after large meals. Diagnosis typically involves a physical examination and imaging studies such as X-rays or endoscopy to visualize the stomach and esophagus. Treatment options include lifestyle modifications, such as weight loss and dietary changes, along with medications to manage symptoms. In more severe cases, surgical intervention may be necessary to repair the hernia and prevent complications like esophageal reflux or strangulation. Recovery from surgery usually involves a few weeks of limited activity, but many patients can return to normal routines relatively quickly. Early diagnosis and management of a hiatus hernia are crucial for improving symptoms and preventing potential complications.

Diaphragmatic Hernia : A diaphragmatic hernia occurs when abdominal contents, such as the stomach or intestines, protrude through a defect or weakness in the diaphragm, the muscular barrier that separates the chest cavity from the abdominal cavity. This condition can be congenital, often present at birth, or acquired due to trauma, surgical complications, or conditions that weaken the diaphragm over time. Congenital diaphragmatic hernias are typically more severe and can lead to respiratory distress in newborns, as the herniated organs can compress the lungs, hindering their development. Symptoms in infants may include rapid breathing, difficulty feeding, and a bluish tint to the skin due to oxygen deprivation. In adults, symptoms may include chest pain, shortness of breath, gastrointestinal issues, or the presence of a noticeable bulge in the abdomen. Diagnosis usually involves imaging studies such as X-rays, CT scans, or ultrasounds, which can help identify the hernia and assess the extent of organ displacement. Treatment typically requires surgical intervention to repair the defect in the diaphragm and reposition any displaced organs back into the abdominal cavity. The surgical approach can vary depending on the size and nature of the hernia, with minimally invasive techniques often preferred when feasible. Recovery times can differ based on the surgical method used and the patient's overall health, but many individuals can resume normal activities within weeks. Timely diagnosis and treatment are crucial to prevent complications such as respiratory distress or obstruction, ensuring better outcomes for affected individuals.
Book An Appointment